The Lancet Diabetes & Endocrinology: Global Commission Proposes Major Overhaul of Obesity Diagnosis
January 15, 2025 · Baton Rouge, LA
Going Beyond BMI to Define When Obesity is a Disease
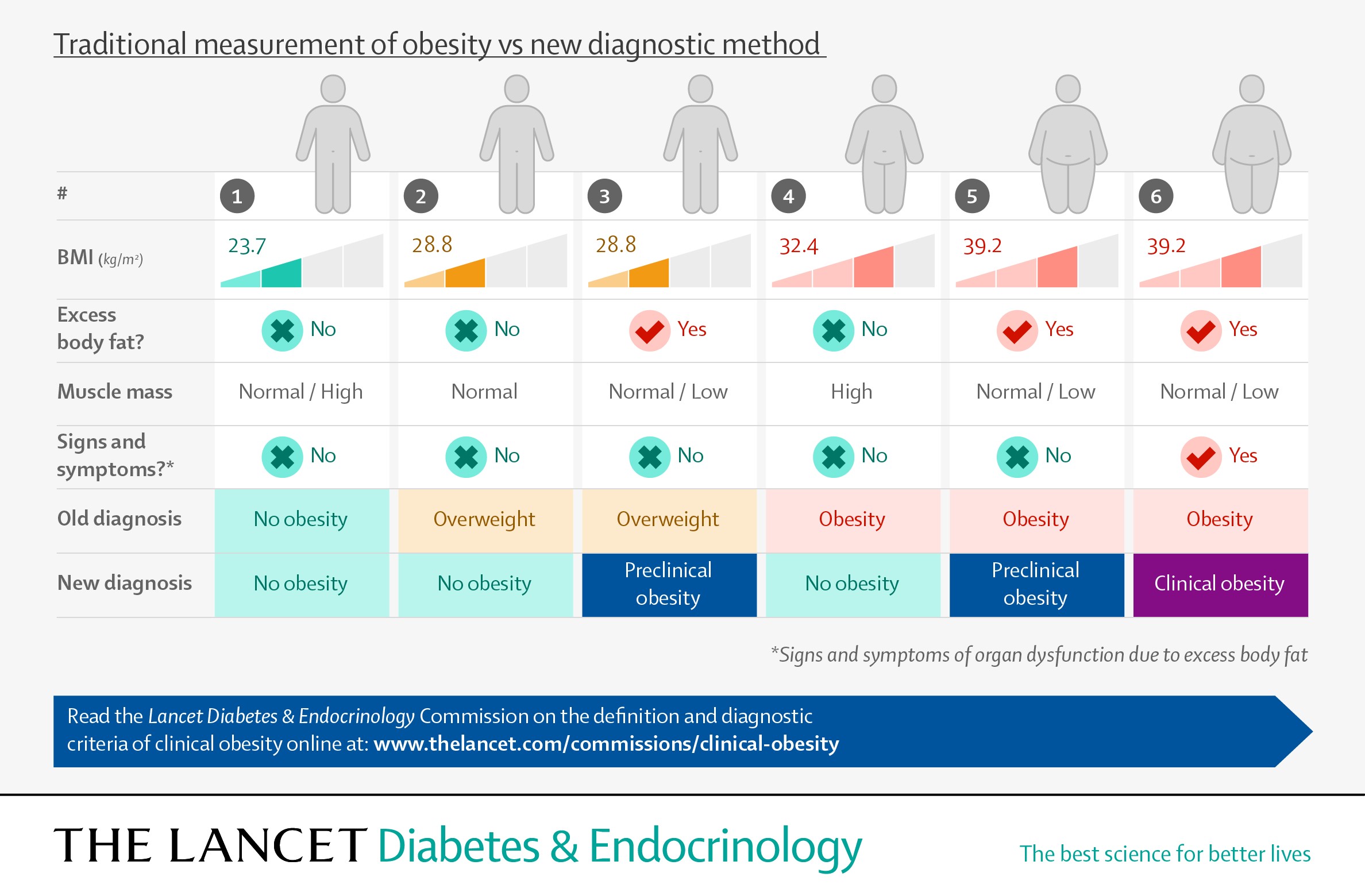
- Current medical approaches to diagnosing obesity rely on BMI which is not a reliable measure of health or illness at the individual level. This can result in misdiagnosis with negative consequences for people living with obesity and wider society.
- The Commission on Clinical Obesity recommends a new, nuanced approach where measures of body fat - for example, waist circumference or direct fat measurement - in addition to BMI are used to detect obesity, therefore reducing the risk of misclassification.
- Additionally, the authors introduce two new diagnostic categories of obesity based on objective measures of illness at the individual level; ‘clinical obesity’ (a chronic disease associated with ongoing organs’ dysfunction due to obesity alone) and ‘pre-clinical obesity’ (associated with a variable level of health risk, but no ongoing illness).
- The Commission authors call for all people living with obesity to receive personalized
health advice and evidence-based care when needed - free of stigma and blame - with
different strategies for clinical obesity and pre-clinical obesity.
 A global Commission, published in The Lancet Diabetes & Endocrinology and endorsed by more than 75 medical organizations around the world [1], presents
a novel, nuanced approach to diagnose obesity, based on other measures of excess body
fat in addition to body mass index (BMI), and objective signs and symptoms of ill
health at the individual level.
A global Commission, published in The Lancet Diabetes & Endocrinology and endorsed by more than 75 medical organizations around the world [1], presents
a novel, nuanced approach to diagnose obesity, based on other measures of excess body
fat in addition to body mass index (BMI), and objective signs and symptoms of ill
health at the individual level.
The proposal is designed to address limitations in the traditional definition and
diagnosis of obesity that hinder clinical practice and healthcare policies, resulting
in individuals with obesity not receiving the care they need. By providing a medically
coherent framework for disease diagnosis, the Commission also aims to settle the ongoing
dispute around the idea of obesity as a disease, which has been at the center of one
of most controversial and polarizing debates in modern medicine.
Commission chair, Professor Francesco Rubino, King's College London (UK) says, “The
question of whether obesity is a disease is flawed because it presumes an implausible
all-or-nothing scenario where obesity is either always a disease or never a disease. Evidence, however,
shows a more nuanced reality. Some individuals with obesity can maintain normal organs’
function and overall health, even long term, whereas others display signs and symptoms
of severe illness here and now.
“Considering obesity only as a risk factor, and never a disease, can unfairly deny
access to time-sensitive care among people who are experiencing ill health due to
obesity alone. On the other hand, a blanket definition of obesity as a disease can
result in overdiagnosis and unwarranted use of medications and surgical procedures,
with potential harm to the individual and staggering costs for society.
“Our reframing acknowledges the nuanced reality of obesity and allows for personalized
care. This includes timely access to evidence-based treatments for individuals with
clinical obesity, as appropriate for people suffering from a chronic disease, as well
as risk-reduction management strategies for those with pre-clinical obesity, who have
an increased health risk, but no ongoing illness. This will facilitate a rational
allocation of healthcare resources and a fair and medically meaningful prioritization
of available treatment options.”
With over one billion people in the world now estimated to be living with obesity
[2], the Commission’s proposal provides an opportunity for health systems globally
to adopt a universal, clinically relevant definition of obesity and a more accurate
method for its diagnosis.
The Lancet Commission on Clinical Obesity was made up of 56 individuals from around the world, including Pennington Biomedical's Dr. John Kirwan, Executive Director and George A. Bray, Jr. Endowed Super Chair in Nutrition; Dr. Eric Ravussin, LSU Boyd Professor and Douglas L. Gordon Chair in Diabetes and Metabolism; and Dr. Philip Schauer, Director of the Metamor Institute and United Companies Life Insurance Co./Mary Kay and Terrell Brown Chair.
Current approaches to diagnosing obesity are ineffective
There is an ongoing debate among clinicians and policymakers over the current diagnostic
approach to obesity, which is prone to misclassification of excess body fat and misdiagnosis
of disease.
Part of the issue is due to obesity being currently defined by BMI, with a BMI of
over 30 Kg/m2 considered as an indicator of obesity for people of European descent. Different, country-specific
BMI cutoffs are also used to account for ethnic variability of obesity-related risk.
Although BMI is useful for identifying individuals at increased risk of health issues,
the Commission highlights that BMI is not a direct measure of fat, does not reflect
its distribution around the body and does not provide information about health and
illness at the individual level.
“Relying on BMI alone to diagnose obesity is problematic as some people tend to store
excess fat at the waist or in and around their organs, such as the liver, the heart
or the muscles, and this is associated with a higher health risk compared to when
excess fat is stored just beneath the skin in the arms, legs or in other body areas.
But people with excess body fat do not always have a BMI that indicates they are living
with obesity, meaning their health problems can go unnoticed. Additionally, some people
have a high BMI and high body fat but maintain normal organ and body functions, with
no signs or symptoms of ongoing illness.” says Commissioner Professor Robert Eckel,
University of Colorado Anschutz Medical Campus (USA).
Beyond Body Mass Index
Whilst recognizing BMI is useful as a screening tool to identify people who are potentially
living with obesity, the authors recommend moving away from detecting obesity based
on BMI alone. Instead, they recommend confirmation of excess fat mass (obesity) and
its distribution around the body using one of the following methods:
- at least one measurement of body size (waist circumference, waist-to-hip ratio or waist-to-height ratio) in addition to BMI
- at least two measurements of body size (waist circumference, waist-to-hip ratio or waist-to-height ratio) regardless of BMI
- direct body fat measurement (such as by a bone densitometry scan or DEXA) regardless of BMI
- In people with very high BMI (e.g. >40 Kg/m2) excess body fat can be pragmatically assumed.
Two new categories of obesity: ‘clinical obesity’ and ‘pre-clinical obesity’
The Commission also provides a new model for disease diagnosis in obesity based on
objective measures of illness at the individual level.
Clinical obesity is defined as a condition of obesity associated with objective signs and/or symptoms
of reduced organ function, or significantly reduced ability to conduct standard day-to-day
activities, such as bathing, dressing, eating and continence, directly due to excess
body fat. People with clinical obesity should be considered as having an ongoing chronic
disease and receive appropriate management and treatments.
The Commission sets out 18 diagnostic criteria for clinical obesity in adults (see
appendix figure 1) and 13 specific criteria for children & adolescents (see appendix
figure 2), including:
- Breathlessness caused by effects of obesity on the lungs
- Obesity-induced heart failure
- Knee or hip pain, with joint stiffness and reduced range of motion as a direct effect of excess body fat on the joints
- Certain alterations of bones and joints in children and adolescents limiting movement
- Other signs and symptoms caused by dysfunction of other organs including kidneys, upper airways, metabolic organs, nervous, urinary and reproductive systems and the lymph system in the lower limbs
Pre-Clinical obesity is a condition of obesity with normal organ function. People living with pre-clinical
obesity therefore do not have ongoing illness, although they have a variable but generally
increased risk of developing clinical obesity and several other non-communicable diseases (NCDs)
in the future, including type 2 diabetes, cardiovascular disease, certain types of
cancer and mental illness, among others. As such, they should be supported to reduce
the risk of potential disease.
“The Commission’s new diagnostic criteria fill a gap in the notion of obesity diagnoses
as they enable clinicians to differentiate between health and illness at the individual
level. We hope that the broad endorsement of the new framework and diagnosis of obesity
by many important scientific societies from around the world will ensure that a systematic
clinical assessment of obesity becomes a requirement in health systems globally,”
says Commissioner Dr. Gauden Galea, WHO Regional Office for Europe.
People living with obesity need personalized care 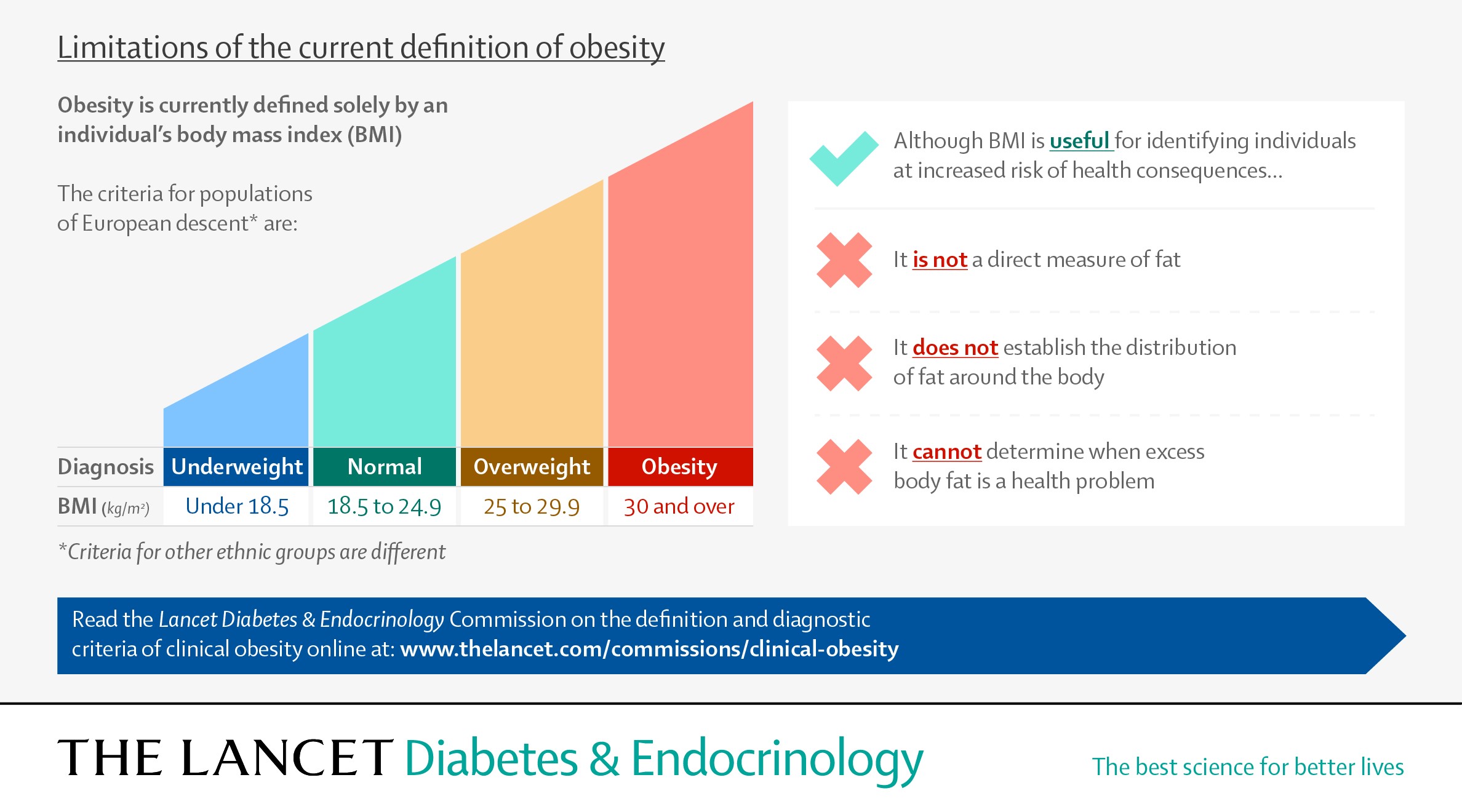 The Commission’s reframing of obesity is designed to ensure that all people living
with obesity receive appropriate health advice and evidence-based care when needed,
with different strategies for clinical obesity and pre-clinical obesity.
The Commission’s reframing of obesity is designed to ensure that all people living
with obesity receive appropriate health advice and evidence-based care when needed,
with different strategies for clinical obesity and pre-clinical obesity.
People with clinical obesity should receive timely, evidence-based treatment, with
the aim to fully regain or improve the body functions reduced by excess body fat,
rather than solely to lose weight. The type of treatment and management for clinical
obesity – lifestyle, medication, surgery, etc –should be informed by individual risk:
benefit assessments and determined by an active discussion with the patient.
Health insurers worldwide often require evidence of other conditions associated with
obesity (e.g. type 2 diabetes) to provide coverage of obesity therapies. As a distinct
chronic illness itself, clinical obesity should not necessitate the presence of another
disease to justify coverage.
People living with pre-clinical obesity are at risk for future diseases but do not
have ongoing health complications due to excess body fat. Accordingly, the approach
to their care should aim at risk-reduction. Depending on the individual level of risk,
this may require just health counselling and monitoring over time, or active treatment
if necessary to reduce substantially high levels of risk.
“This nuanced approach to obesity will enable evidence-based and personalised approaches
to prevention, management and treatment in adults and children living with obesity,
allowing them to receive more appropriate care, proportional to their needs. This
will also save healthcare resources by reducing the rate of overdiagnosis and unnecessary
treatment,” says Commissioner Professor Louise Baur, University of Sydney (Australia).
The Commission involved 56 world leading experts across a broad range of medical specialties,
including endocrinology, internal medicine, surgery, biology, nutrition and public
health, representing many countries and diverse healthcare systems. The Commission
also included people living with obesity and specifically considered the potential
impact of the new definitions of obesity on widespread societal stigma.
"Studies show that the way obesity is usually talked about adds to weight stigma,
making it harder to prevent, manage and treat. The approach proposed by this Commission
can help clear up misconceptions and reduce stigma. We also urge better training for
healthcare workers and policymakers to tackle this issue," says Joe Nadglowski, patient
advocate and Commissioner, Obesity Action Coalition (USA).
NOTES TO EDITORS
There was no industrial grants or other funding for this initiative. King’s Health
Partners hosted the initiative and provided logistical and personnel support to facilitate
administrative work and the delphi-like consensus-development process. For a full
list of researchers and their institutions see the Commission report.
The Commission will be launched at a public livestreamed event from 1-5 pm GMT (7-11am
CST) on Thursday, Jan. 16. Register here for the Lancet feed or details on the launch event being held at Pennington Biomedical are available
at https://www.pbrc.edu/news/media/2025/lancetadvisory.aspx.
References:
[1] For a full list of medical organisations endorsing the Commission see appendix
2 (pp 2–3).
[2] https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(23)02750-2/fulltext
Resources from the World Obesity Federation to support discussing obesity in the media:
- The do’s and don’ts when talking about obesity
- Image use and obesity: recommendations
- Visit worldobesity.org/resources/image-bank for a selection of free to download images available for use.
The labels have been added to this press release as part of a project run by the Academy
of Medical Sciences seeking to improve the communication of evidence. For more information,
please see: http://www.sciencemediacentre.org/wp-content/uploads/2018/01/AMS-press-release-labelling-system-GUIDANCE.pdf if you have any questions or feedback, please contact The Lancet press office pressoffice@lancet.com
For interviews with the authors, please contact h.taylorlewis@lancet.com. For interviews with commissioners from Pennington Biomedical Research Center, please
contact ernie.ballard@pbrc.edu.
Contact The Lancet press office:
LONDON
Hannah Taylor Lewis, Senior Media and Communications Manager
Tel: +44 (0) 7553 575923
h.taylorlewis@lancet.com
Seil Collins, Head of Media and Communications
Tel: +44 (0) 7787 222936
seil.collins@lancet.com
USA
Johanna Harvey, Deputy Head of Media and Communications, North America
Tel: +1 267-515-1767
johanna.harvey@lancet.com
OUTSIDE OF UK HOURS
Tel: +44 (0) 207 424 4249
For more information contact:
Joe Coussan, Media Relations Manager, joe.coussan@pbrc.edu, 225-763-3049 or Ernie Ballard, Senior Director of Communications & Marketing, ernie.ballard@pbrc.edu, 225-263-2677.
About the Pennington Biomedical Research Center
The Pennington Biomedical Research Center is at the forefront of medical discovery as it relates to understanding the triggers of obesity, diabetes, cardiovascular disease, cancer and dementia. Pennington Biomedical has the vision to lead the world in promoting nutrition and metabolic health and eliminating metabolic disease through scientific discoveries that create solutions from cells to society. The Center conducts basic, clinical and population research, and is a campus in the LSU System.
The research enterprise at Pennington Biomedical includes over 600 employees within a network of 44 clinics and research laboratories, and 16 highly specialized core service facilities. Its scientists and physician/scientists are supported by research trainees, lab technicians, nurses, dietitians and other support personnel. Pennington Biomedical is a globally recognized state-of-the-art research institution in Baton Rouge, Louisiana. For more information, see www.pbrc.edu.
Pennington Biomedical Research Center
6400 Perkins Road
Baton Rouge, LA 70808