You use your cellphone every day. What if it could help you lose weight?Faculty Feature: Get to Know Dr. Corby Martin

Walk into a restaurant; grab a table; order food. Before you eat, pull out your phone to snap a photo of your plate.
That process probably sounds familiar if you're like most people who own a smartphone.
However, food photos hold much more potential than a Snapchat story. In fact, with the right technology, quick snapshots can provide accurate estimates of the caloric content of a meal.
Scientists at LSU's Pennington Biomedical Research Center are exploring the potential of mobile health platforms to help people live healthier lives.
When gadgets and devices are touted as health's arch nemesis, it's easy to take an anti-screen time stance. But with technology so integrated into every aspect of life, it isn't practical.
"Technology is here to stay, and we need to leverage it to promote our health," said Dr. Corby Martin, director of the Ingestive Behavior, Weight Management & Health Promotion Laboratory at Pennington Biomedical.
Now that mobile devices are commonplace, the goal is to make people's devices more helpful than harmful, Martin said.
The Remote Food Photography Method (RFPM) is an example of Martin's work. He developed the concept after clinical research exposed a critical issue: People are terrible at gauging portion sizes.
"The difference between what people think they've eaten and what they've actually eaten is enough to sabotage weight-loss efforts," Martin said. "All of us, even the healthiest of people, need help with this."
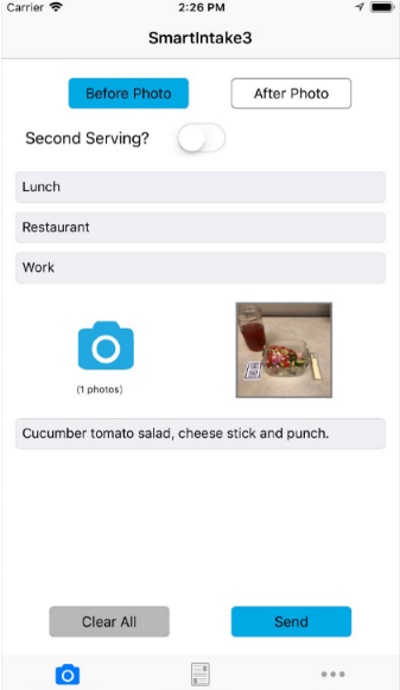
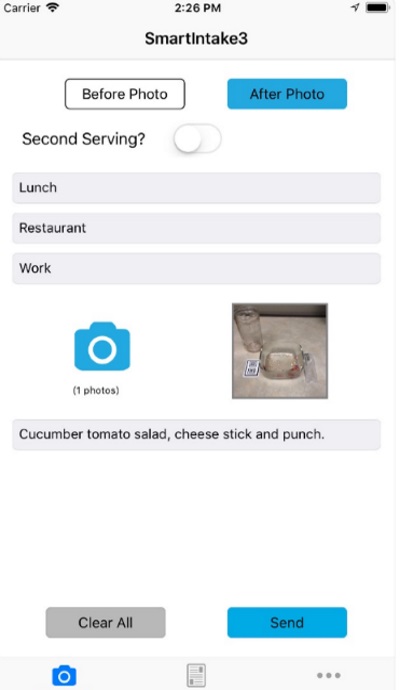
Two examples of Martin's work are the SmartIntake app, available for free download on the App Store for iOS devices, and the SmartLoss website, which can be used on any device with Internet. Though the two services are up and running, users must be working with a Pennington Biomedical clinician to get full use of the systems.
SmartIntake is used to estimate the energy, or caloric, intake of app users. It works by prompting participants to take before and after photos of their meals and submit the photos to a server maintained by scientists working on the app.
The system is successful because the participants' food photos are analyzed by dietitians, who can then counsel participants about how to meet their daily nutritional goals.
What's particularly important is that the food-intake data are collected in real-time, everyday environments, rather than in a lab.
Self-report methods such as food diaries and 24-hour recalls are commonly used to estimate food intake, Martin said. But people tend to inaccurately estimate portion size when using these methods. This contributes to people underestimating their caloric intake by around 35 percent.
In the initial SmartIntake study, Martin said 94 percent of participants preferred the RFPM to pen-and-paper food diaries. It is hoped that such apps can help people stick to their diets better.
"When it comes to measuring what people eat, a picture really is worth a thousand words," Martin said. "Further, the images are captured and transmitted to researchers or clinicians right when we are eating, which can increase accountability."
After finding success with SmartIntake, Dr. Martin and colleagues, including Drs. Leanne Redman and Diana Thomas, began developing SmartLoss, which creates a virtual weight-loss experience.
The mobile health platform consists of two elements: A clinician dashboard for health professionals and a smartphone app for participants.
The app connects to a WiFi-enabled bathroom scale and accelerometer. Those features allow the app to collect client information such as changes in body weight and physical activity patterns.
Data from the individual, such as starting body weight, body composition, current activity patterns, and goals, are used to guide personalized recommendations regarding weight loss and behavior change.
The clinician dashboard allows professionals to easily and remotely monitor clients, which allows for timely treatment and continuous data collection.
Martin said mobile health approaches are critical to reaching people with limited access to care. Further, they promise to be more cost-effective than traditional care for chronic conditions such as obesity and diabetes, though additional research is needed in this area.
To have the advice and encouragement of a doctor, dietitian, coach, trainer or any health professional at the push of a button is a luxury unheard of 10 or 20 years ago.
"The world is changing, and health care needs to change with it," Martin said. "We need to optimize the potential of mobile health."
Most recently, Martin and Dr. John Apolzan received a grant from the LSU Board of Supervisors (the Leverage Innovation for Technology Transfer program) for PortionSize: A market-ready app to estimate and manage portion size.
The new app is still in the development stage. Be the first to get updates on PortionSize by signing up for our email newsletter.
Interested in participating in a clinical trial? See our currently enrolling studies here.
If you'd like to receive e-mail updates about our other ongoing and upcoming studies, sign up here.
|
|
For more information on how you can support this and other projects at LSU’s Pennington Biomedical Research Center, visit www.pbrf.org.


