Covid-19 Resource Center
Reviewed 03/14/2022
As part of Pennington Biomedical's response to the global pandemic, this COVID-19 Resource Center has been created for you to stay informed about the Center’s reaction and operations during this unprecedented time. Resources for participants, employees, researchers and the general public can be found in this center.
Free Vaccine sites : covidvaccine.la.gov or call 1-855-453-0774 to schedule a vaccine appointment.
News & Resources
Dwindling Cases, Hospitalizations Prompt Governor to Lift COVID Emergency Order
March 14, 2022
For the first time in 24 months, Gov. John Bel Edwards will not renew his COVID public health emergency order.
“I want to be clear that just because the proclamation is expiring doesn’t mean COVID is over. If the circumstances call for it, I will not hesitate to declare another emergency,” Edwards said. “God willing, we will never have to see such difficult mitigation measures in our state again. Thankfully, at this time, we are no longer in a crisis. I don’t know what the future holds, but I do know that we are in a much better place today than we were two years ago.”
Edwards signed the emergency order on March 11, 2020, three days before the first person in Louisiana died from COVID-19. In the two years since, more than 16,900 Louisianans have died from the virus.
However, the state and country have recently seen significant drops in cases and hospitalizations, Edwards said. Unlike two years ago, safe and effective vaccines are widely available. The Centers for Disease Control and Prevention’s community-risk models show most of Louisiana’s parishes have a low risk for COVID spread.
Read more here.
As COVID declines, Pennington Biomedical Makes a Cautious Return to More Normal Activities
Feb. 28, 2022
As COVID-19 cases are continuing to decline, Executive Director Dr. John Kirwan said
the Research Center is modifying its protocols to allow for a cautious return to normal
for Center activities, effective immediately.
Meetings/Gatherings – Meetings are allowed at 100 percent of the meeting-room capacity
Masking – Masks are recommended for indoor gatherings of greater than 10 people. Masks are
still required in situations involving close interactions with participants in clinical
areas. If you wish to continue to wear a mask, you may certainly do so.
Testing – Employees who are subject to mandatory testing will now be required to test once
per week each Monday. Anyone who tests positive or has been exposed should reach out
to Celeste Waguespack, our Infection Control Officer. COVID-19 PCR testing is available
to employees and their immediate household for those who qualify based on CDC guidance.
Please contact Celeste Waguespack for further information and a link to the testing
form.
"It is everyone’s responsibility to help keep Pennington Biomedical a safe place to
work," Dr. Kirwan said. "If you are feeling ill, stay home. Do your part by continuing
to use best practices of frequent hand-washing, keeping work surfaces clean, and wearing
masks as recommended."
If you have not received your vaccination booster, I strongly encourage you to protect
yourself, your family, friends, community, and co-workers by doing so.
As Omicron Surges, Gov. Edwards, LDH Urge People to Celebrate at Home
Dec. 30, 2021
Amid record numbers of COVID-19 cases and soaring hospitalizations, the governor and health officials urged Louisiana residents to celebrate New Year’s Eve at home and released new return-to-school recommendations for K-12 students.
The Omicron variant is driving the fifth surge in coronavirus cases, Gov. John Bel Edwards said. On Wednesday, Louisiana set a new record with 9,378 new cases. On Thursday, Louisiana broke that record with 12,467 new cases.
In addition, the number of Louisianans hospitalized has jumped 268 percent since Dec. 16, and the vast majority of those people have not been fully vaccinated.
“I’m very sorry that we’re back here,” Edwards said. “Unfortunately, we don’t get a vote in what this virus does, but we do get a choice on how we respond…. I strongly encourage you to join me in modifying your plans this New Year’s Eve and not gathering with people outside of your immediate household.”
However, Edwards said he is encouraged by the fact that more Louisiana residents – nearly 72,000 this month – are choosing to get the COVID-19 vaccine.
The Health Department’s Guidance and Recommendations during the Omicron surge, also
include:
• Get vaccinated and boosted, if eligible, to protect yourself and others.
• Mask regardless of vaccination status. Mask in indoor public places; mask indoors
when with people outside your everyday household; and mask outdoors when distancing
is not possible.
• Limit exposure to those outside your everyday household.
• Work remotely if possible.
The K-12 Return-to-School Recommendations include:
• Mask universally indoors and outside when socially distancing is not possible. Maintain
a distance of at least 6 feet during mealtimes when masking is not possible.
• Most outbreaks identified in school settings have been associated with extracurricular
activities. It is safest to suspend extracurricular activities while the extremely
transmissible Omicron variant is circulating at such high levels (until statewide
incidence is below 200 infections per 100,000 people).
• Do not participate in social gatherings with individuals outside your everyday household
(e.g., pep rallies, school dances) until statewide incidence is below 200 infections
per 100,000 people.
• Get vaccinated and boosted when eligible.
• Children should be tested prior to the return to school.
While at-home antigen tests remain in short supply, PCR tests are free, widely available and more sensitive when it comes to detecting the Omicron. PCR test results are typically available within 24-48 hours.
The Health Department’s Other Testing Advice includes:
• Remember that tests are a snapshot in time, and a negative test does not mean you
will not test positive later if you were exposed to the virus.
• Do not visit an emergency room to obtain a test. Emergency rooms are for the seriously
ill or someone needing immediate medical attention.
To read more, click here.
As Omicron Spreads, Governor Extends Public Health Emergency Order, Requires Masking
in Most State Agencies
Dec. 23, 2021
The rapid spread of the Omicron variant prompted Gov. John Bel Edwards to extend the state’s public health emergency order requiring face masks to be worn inside state agencies.
Around 50 percent of Louisianans have already been vaccinated, and more than 460,000 Louisianans have already taken a booster.
“Now more than ever it is important that everyone get vaccinated or, if they are eligible, take a COVID booster. The vaccines are safe, effective and widely available …. We know from the most recent CDC data that unvaccinated people are 10 times more likely to test positive for COVID and 20 times more likely to die from COVID than fully vaccinated people who also have gotten their booster shots,” Gov. Edwards said. “Simply put, one of the riskiest things you can be in Louisiana right now is unvaccinated. You’re signing up for the potential of severe illness, hospitalization or something even worse. We have seen how previous COVID surges have torn through our state and none of us wants to go back to the days of August and September, when thousands of people were hospitalized and dying.”
To read more, click here.
LDH Recommends Coronavirus Boosters for All Adults
Nov. 19, 2021
The Louisiana Department of Health has recommended booster doses for every fully vaccinated adult in the state.
A person is considered fully vaccinated if they have gotten two doses of the Pfizer or Moderna vaccine, or one dose of the Johnson & Johnson vaccine.
“By working together, we have made significant progress in slowing the spread of COVID-19 in our state, which is why as we head into the holiday season it is critical that Louisianans get a booster shot as soon as they become eligible in order to protect themselves and their loved ones against the possibility of another surge,” said Gov. John Bel Edwards. “
The following individuals are now eligible and recommended to receive a booster dose:
- Anyone 18 and older who completed their two-dose Pfizer or Moderna vaccine series 6 or more months ago.
- Anyone 18 and older who received their one-dose Johnson & Johnson vaccine two or more months ago.
Read more about the Health Department’s recommendation here.
CDC Recommends Pfizer COVID-19 Vaccine for Children 5-11
Nov. 3, 2021
Children ages 5 to 11 may now get Pfizer’s COVID-19 vaccine.
The U.S. Centers for Disease Control and Prevention’s approval expands vaccine recommendations to more than 28 million children nationwide and around 450,000 in Louisiana.
COVID-19 cases in children have resulted in hospitalizations, deaths, MIS-C (inflammatory syndromes) and long-term complications, such as “long COVID,” in which symptoms can linger for months. COVID-19 cases in children surged throughout the summer as the Delta variant spread. During the six weeks from late June to mid-August, the number of children and adolescents hospitalized by COVID-19 jumped 400 percent.
The children's dose of the Pfizer vaccine is one-third of the adult dose. Vaccine clinics, children's hospitals and pediatricians' offices across the country have received or are receiving shipments of the vaccine. Experts say vaccinations should begin as early as this week.
Read more about the CDC decision here.
FDA Approves Moderna, Johnson & Johnson Boosters, Mixing COVID Vaccines
Oct. 21, 2021
Americans who got the Moderna or Johnson & Johnson vaccines are eligible for COVID-19 booster shots, and they can choose whatever brand they prefer for their next dose.
The U.S. Food and Drug Administration’s decision expands eligibility for the boosters to tens of millions of people. Regulators say “mixing and matching” vaccines makes it simpler for the vaccinated to get another dose. In addition, people who wanted to get a booster but hesitated because they had a side effect or effects from their initial shots can now choose another brand.
Specifically, the FDA is authorizing a third Moderna shot for seniors and others at high risk from COVID-19 because of their health, jobs or living conditions if it has been six months since their last shot.
Meanwhile, everyone who got the Johnson & Johnson single-shot vaccine, no matter their age, can get a second dose if it has been two months since their initial vaccination.
Read more about the FDA decision here.
Shot for 100 Campaign Expands to Anyone in Louisiana Who Gets COVID Vaccine
Oct. 1, 2021
Louisiana’s Shot For 100 vaccine incentive program expanded Friday to include anyone in Louisiana who gets their first COVID vaccine. Patients must receive the vaccine at participating community-based sites as listed on ShotFor100.com.
Anyone receiving their first shot is eligible and may only participate once. Minors are eligible for the cash incentive but require parental consent to get the vaccine. The program was originally limited to college students.
"By expanding the Shot for 100 campaign to everyone in Louisiana, we hope to see tens of thousands of additional people get their first dose of the safe and effective COVID vaccines, so we can end this pandemic once and for all,” Gov. John Bel Edwards said. “If you’ve not yet been able to go Sleeves Up yet, we’re hoping a cool $100 will help make the decision easier."
Individuals will receive a deactivated Visa gift card upon vaccination. After registering online at ShotFor100.com, the card will be loaded with $100. This limited-time offer for college students and the general public will end October 30 or while supplies last.
Read more here.
Pfizer Booster Shots Are Now Available to Adults at Increased Risk, Following New
CDC Guidance
Sept. 24, 2021
Millions of Americans at the highest risk for COVID-19 may receive a Pfizer-BioNTech booster shot to help increase their protection, following new guidance from the Centers for Disease Control (CDC).
The CDC also recommended booster shots for people in high-risk work and institutional settings.
"We welcome and adopt here in Louisiana the new FDA and CDC guidance making booster shots of the Pfizer vaccine available to adults at increased risk," said Dr. Joseph Kanter, State Health Officer. "The deliberations by both federal health agencies this past week reaffirmed that the vaccines are safe and effective, and they are everyone's best protection against COVID hospitalization and death. That's why our number one priority remains helping more Louisianans get their first shots."
If you are 6 months out from your two-dose Pfizer series, you are now eligible to receive a booster shot if you are:
- Age 65 or older
- Age 18 or older and have one of many underlying medical conditions
- Age 18 or older and live or work in a setting that places you at risk of being exposed to COVID
As always, LDH recommends you discuss your individual situation and risk/benefit analysis with your doctor or medical practitioner.
State, Federal Officials Applaud FDA Approval of Pfizer COVID-19 Vaccine
Aug. 23, 2021
State and federal health officials applauded the U.S. Food and Drug Administration's full approval of Pfizer’s COVID-19 vaccine, calling it a historic moment in fighting the virus.
“This full FDA approval of the first COVID vaccine follows months of clinical trials and millions upon millions of real-world doses safely administered across the globe. This vaccine is well researched, very safe and highly effective at preventing serious COVID illness, hospitalization and death,” Gov. John Bel Edwards said. “It is my fervent hope that any Louisianan who was waiting for the FDA approval of the vaccine will take action to immediately receive their shot."
More than 2.2 million Louisianans have taken at least one dose of the vaccines that are available statewide. Edwards said he is optimistic that those numbers will grow as the state's residents fight together to end the pandemic.
Acting FDA Commissioner Janet Woodcock, M.D., said although millions of people have already safely been vaccinated, the FDA approval may instill more confidence in COVID-19 vaccines.
"Today’s milestone puts us one step closer to altering the course of this pandemic in the U.S.,” she said.
Monoclonal Antibodies Show Promise, Could Prevent COVID Hospitalizations, Gov. Edwards
Says
Aug. 20, 2021
Infusions of monoclonal antibodies, if given shortly after a person is infected with COVID-19, can help prevent the person from being hospitalized, Gov. John Bel Edwards said Friday.
The treatment is effective and could help prevent the state’s hospitals from being overwhelmed by coronavirus cases, Edwards said. Health officials are trying to get the treatment in as many hospitals as possible. But the main goal is to prevent people from getting COVID if at all possible, and the current surge is not slowing.
“We continue to report astronomical numbers of cases across the state of Louisiana. Today, 5,922 new cases of COVID, and very sadly, we’re also reporting 67 new deaths across the state of Louisiana,” Edwards said.
There was a little good news, he said. The number of Louisiana residents hospitalized did not set a record for the second day in a row,
However, the Delta variant’s impact – it accounts for close to 100 percent of the cases – remains troubling, especially among children, who now account for 28 percent of all COVID cases.
More cases were reported during the first week of school than any week of the previous school year, Edwards said.
Read more here.
Federal Health Department Will Make COVID-19 Booster Shots Available in Fall
Aug. 18, 2021
The U.S. Department of Health and Human Services will begin offering COVID-19 booster shots in the fall.
The available data make very clear that protection against COVID-19 infections decreases over time following the initial doses of vaccination, said Dr. Rochelle Walensky, Director of the Centers for Disease Control and Prevention. In addition, with the Delta variant, health officials have begun to see reduced protection against mild and moderate disease.
“We are prepared to offer booster shots for all Americans beginning the week of September 20 and starting eight months after an individual’s second dose. At that time, the individuals who were fully vaccinated earliest in the vaccination rollout, including many health care providers, nursing home residents, and other seniors, will likely be eligible for a booster,” Walensky said.
Two additional steps are necessary before the shots can be made available.
- The Food and Drug Administration must independently evaluate and determine the safety and effectiveness of a third dose of the Pfizer and Moderna mRNA vaccines.
- The CDC’s Advisory Committee on Immunization Practices must issue booster dose recommendations based on a thorough review of the evidence.
Federal officials said booster shots will likely be needed for people who received the Johnson & Johnson vaccine.
“Our top priority remains staying ahead of the virus and protecting the American people from COVID-19 with safe, effective, and long-lasting vaccines especially in the context of a constantly changing virus and epidemiologic landscape,” Walensky said.
Read more here.
COVID-19 Vaccines for Moderately to Severely Immunocompromised People
Aug. 17, 2021
CDC now recommends that people whose immune systems are compromised moderately to severely should receive an additional dose of mRNA COVID-19 vaccine after the initial 2 doses. Widespread vaccination is a critical tool to help stop the pandemic. Read CDC’s statement.
What You Need to Know
- People who are moderately to severely immunocompromised are especially vulnerable to COVID-19 because they are more at risk of serious, prolonged illness.
- People with moderately to severely compromised immune systems may not build the same level of immunity to 2-dose vaccine series compared to people who are not immunocompromised.
- People who have compromised immune systems may benefit from an additional dose to make sure they have enough protection against COVID-19.
- CDC recommends people who are moderately to severely immunocompromised should receive an additional dose of mRNA COVID-19 vaccine after the initial 2 doses.
- This additional dose intended to improve immunocompromised people’s response to their initial vaccine series is not the same as a booster dose, given to people when the immune response to a primary vaccine series is likely to have waned over time
Read more here.
Latest COVID-19 Surge Threatens to Overwhelm Louisiana Hospitals
Aug. 13, 2021
Gov. John Bel Edwards and health officials warned that the ongoing flood of COVID-19 cases could soon swamp hospitals already struggling to find enough beds and staff to treat the most seriously ill patients.
“The problem we have right now isn’t that these are the highest number of cases and percent positivity and hospitalizations and so forth we’ve ever had in the state. They are that,” Edwards said. “They are the highest in the country. And if the state of Louisiana were an independent nation, we would be among the highest in the world. “
Nobody should wait to get vaccinated, he said. There are more than 1,400 health care providers able to provide vaccines, and finding a site is as easy as dialing 211.
The number of Louisiana residents hospitalized because of COVID-19 swelled to a record 2,907 on Friday. But health officials expect the record won’t last long. Confirmed COVID-19 cases increased by 17 percent this week, the fastest rate of the pandemic so far.
Dr. Amanda Logue, the chief medical officer of Ochsner Lafayette General, said the hospital workers are beyond exhausted, and the pandemic is worse than ever before.
She and other health officials called on Louisiana residents to get vaccinated and to wear masks.
Edwards agreed.
“We’ve got to slow Delta down. We have to slow the transmission. We have to slow the hospitalizations, and Lord knows we have to reduce the number of deaths that we are reporting every day,” Edwards said.
Read more here.
Delta Variant-Driven COVID-19 Surge Worsens, Threatens to Overwhelm Hospitals. Gov.
Edwards, State Health Officials Urge Residents to Mask Up, Get Vaccinated
Aug. 6, 2021
The fourth surge of COVID-19 shows no sign of slowing and may not peak until mid-September,
a situation state health officials described as “terrifying.”
“There is no tangible evidence that we are changing the trajectory of the virus, which
is quite frankly terrifying,” Dr. Joseph Kanter, State Health Officer, said Friday.
The latest numbers for Louisiana show 11,210 residents have died from COVID-19; 2,421
residents are now in hospitals; and the total number of cases has grown to 573,903.
Some 50 hospitals have asked the state for assistance to cope with patients flooding
their facilities.
Gov. John Bel Edwards said Louisiana’s latest and worst wave of infections could have
been prevented with more indoor masking and vaccinations. Those are now the two
most powerful tools at our disposal, he said.
However, Edwards said he was encouraged to see that many of the people now seeking
vaccinations had changed their minds about getting the vaccines. It doesn’t matter
why you didn’t get vaccinated before, he said. What matters is that you get vaccinated
now.
Read more here.
Gov. Edwards Temporarily Reinstates Statewide Mask Mandate amid Skyrocketing COVID-19
Cases
Aug. 2, 2021
Gov. John Bel Edwards temporarily reinstated an indoor mask mandate for people age five and older, citing “increasingly alarming” and “heartbreaking” numbers of COVID-19 cases, hospitalizations and deaths.
“We’re the worst in the country in terms of this COVID surge, and that is because of the Delta variant, which is a game changer, and the fact that quite frankly, not enough people have been vaccinated in Louisiana,” Edwards said.
The mandate goes into effect on Wednesday for everyone, vaccinated or unvaccinated, when indoors or in public. However, Edwards urged residents not to wait until Wednesday.
The virus will continue spreading until then, he said. The mandate will remain in effect until at least Sept. 1.
Edwards cited data from the Centers for Disease Control and Prevention that shows that vaccination reduces one’s chance of becoming infected with COVID-19, but those who do become infected with the Delta variant despite being fully vaccinated are likely at risk of transmitting it to others.
Read more here.
Gov. John Bel Edwards May Implement Another Mask Mandate
July 30, 2021
Gov. John Bel Edwards warned Friday he is “seriously considering” another indoor mask mandate for everyone in Louisiana, whether vaccinated or unvaccinated, as COVID-19 hospitalizations and deaths ballooned to record levels.
The Louisiana Department of Health today reported 5,313 new COVID-19 cases with a positivity rate of about 13.35 percent on new tests, and 30 new deaths and 1,740 hospitalizations from the virus. Those not fully vaccinated account for around 90 percent of the cases and hospitalizations, and 85 percent of the deaths.
Hospital leaders throughout the state are urging the governor to reinstate the indoor mask mandate, he said. COVID-19 conditions have become more drastic, which means the state will have to change its approach.
LDH Medical Director Dr. Joseph Kanter said one person infected with the Delta variant will infect six to 10 other people.
Louisiana needs to mask up and get vaccinated to stem the spread of the virus and to save its residents’ lives, Edwards said.
There are breakthrough cases of COVID among the vaccinated, he said. But vaccines prevent the most serious effects so “run, don’t walk to get your vaccine.”
Interim Public Health Recommendations for Fully Vaccinated People
July 28, 2021
The Centers for Disease Control and Prevention have updated the guidance for fully vaccinated people to reflect the impact of the Delta variant.
To protect yourself and others, the CDC recommends:
- Wearing a mask in public indoor settings in areas of substantial or high transmission.
- Wearing a mask is most important if you or someone in your household are unvaccinated, have a weakened immune system, or have an underlying medical condition that puts you or them at increased risk for severe disease.
- If you have a known exposure to someone with suspected or confirmed COVID-19, get tested within 3-5 days after exposure, and wear a mask in public indoor settings for 14 days or until they receive a negative test result.
- Universal indoor masking for all teachers, staff, students, and visitors to schools, regardless of vaccination status.
Read more here.
Gov. John Bel Edwards Recommends All Louisianans Wear Masks Indoors for the Duration of Louisiana’s Fourth
COVID Surge
July 23, 2021
With COVID-19 cases surging, Gov. John Bel Edwards and the state Department of Health recommended that all people, both vaccinated and unvaccinated, wear masks indoors when social distancing is not physically possible.
Updated LDH guidance on masking, testing for vaccinated people and workplace accommodations is part of the state’s strategy for ending its fourth surge of COVID, along with increasing Louisiana’s vaccination rate. Additional measures may be announced later if the situation worsens.
“The White House has notified Louisiana that we are a State of Concern because we are the leading edge of the COVID-19 surge, due to the rapid spread of the Delta variant among the unvaccinated in our state,” Edward said. “Indeed, Louisiana leads the nation in case growth, with 47 cases per capita. This should come as no surprise to anyone who has watched our case counts and hospitalizations continue to climb, and it necessitates additional guidance for how all people should stay safe in Louisiana right now, including wearing masks indoors, when unable to maintain social distancing, testing after suspected exposure even if they are vaccinated and, if possible, working remotely from home to limit exposure to groups.”
Read more here.
Gov. John Bel Edwards Encourages All Louisianans to Take Precautions with Surge in
COVID-19 Cases Among the Unvaccinated
July 16, 2021
With COVID-19 cases, hospitalizations and deaths surging among unvaccinated Louisianans, Gov. John Bel Edwards urged state residents who have not been vaccinated to get the vaccine.
Between February and July of 2021, unvaccinated people in Louisiana were 20 times more likely to become ill with COVID-19.
“The Delta variant of COVID is now the dominant strain in Louisiana and without the protection that the safe and effective vaccines offer, you are far more likely to become ill with COVID in Louisiana. Our hospitals are again stretched thin with limited staff capacity, and the vast majority of COVID patients are not yet fully vaccinated against the illness,” Edwards said.
Read more here.
CDC Data Tracker Weekly Review Newsletter Updates COVID-19 Variants Report, Including
Delta Variant
June 28, 2021
The most recent CDC Data Tracker Weekly Review newsletter reports the B.1.617.2 (Delta)* variant was classified as a Variant of Concern (VOC) on June 15th because it spreads from person to person more easily than other variants and may cause more severe disease. The current vaccines still prove to be effective protection against transmission of the Delta variant, reinforcing the recommendations to get vaccinated. The CDC also advises to follow state and local health official guidance on social distancing and masking precautions against transmittal.
Get Your "Shot at $1 Million" and More Cash and Scholarship Prizes by Entering the
COVID-19 Vaccine Lottery
June 18, 2021
Fourteen vaccinated Louisianans will win scholarships and cash prizes – including one adult who will win $1 million – throughout July as part of the Shot At A Million campaign the state is launching to reward residents who have taken or who choose to get their COVID-19 vaccine, Gov. Edwards announced Thursday.
Entries begin Monday, June 21st at 12 PM through ShotAtAMillion.com or by calling 877-356-1511.
Any resident who has taken at least one COVID vaccine dose can register to win.
- Enter by July 9, 2021 by 11:59 p.m. CDT for the July 14 drawing
- Enter by July 16, 2021 by 11:59 p.m. CDT for the July 21 drawing
- Enter by July 23, 2021 by 11:59 p.m. CDT for the July 28 drawing
- Enter by July 30, 2021 by 11:59 p.m. CDT for the August 4 drawing
- Enter by July 31, 2021 by 11:59 p.m. CDT for the August 4 Grand Prize Drawing
Delta Variant More Contagious, Vaccines Still Protect Against It
6/14/2021
The Delta variant of the coronavirus is more contagious than the Alpha variant and current data indicates it seems to lead to more hospitalizations. Good news: The current vaccines prove the be effective protection against transmission.
Gov. John Bel Edwards Follows Updated CDC Guidance and Removes Mask and Social Distancing
Recommendations for Individuals Fully Vaccinated Against COVID-19
May 14, 2021
Daily life is returning to normal for many in Louisiana as Gov. John Bel Edwards revises Louisiana's COVID-19 mask guidance for those who are fully vaccinated. Following Centers for Disease Control recommendations, the Governor's revised proclamation provides that "fully vaccinated people no longer need to wear a mask or physically distance except in certain limited situations."
The limited situations that still call for mask use and distancing detailed in Gov. Edwards' announcement include mass or public transit, health care facilities and correctional institutions.
"Based on what we know about COVID-19 vaccines, people who have been fully vaccinated can start to do some things that they had stopped doing because of the pandemic," CDC website, 5/14/2021.
Pfizer COVID-19 Vaccine Now Available to All Louisiana Residents Ages 12 and Above
May 13, 2021
Gov. John Bel Edwards announced today that Louisianans ages 12 and up can now receive the COVID-19 vaccine. The recommendation follows the Centers for Disease Control and Prevention actions on Wednesday and the Food & Drug Administration (FDA) emergency use authorization earlier this week.
If you haven't been vaccinated yet, you can locate sites in Louisiana at the Department of Health website covidvaccine.la.gov or call 1-855-453-0774 to schedule a vaccine appointment.
Updated Janssen COVID-19 Vaccine Frequently Asked Questions
MedWatch - The FDA Safety Information and Adverse Event Reporting Program
April 14, 2021
The FDA and CDC are reviewing data involving six cases reported to the Vaccine Adverse Event Reporting System (VAERS) of a low level of platelets in the blood in combination with a rare and severe type of blood clot called cerebral venous sinus thrombosis (CVST) in individuals who had received the Janssen COVID-19 Vaccine. One individual died. All cases occurred in females ranging in age from 18 through 48 years. In some of the reported cases of CVST, blood clots also involved large veins in the abdomen.
Out of an abundance of caution, the FDA and CDC are recommending a pause in the use of the Janssen COVID-19 Vaccine while the FDA and CDC, including through its Advisory Committee on Immunization Practices investigate these reports of serious adverse events.
Read more here including who is at risk for adverse events and what should health care providers look for in evaluating Janssen COVID-19 Vaccine recipients for the rare adverse events.
COVID-19 Vaccines: Things to know
March 2, 2021
The Centers for Disease Control has compiled a list of key facts and myth busters about the Covid-19 vaccines. It is frequently updated with the latest highlights that are scientifically verified and approved for distribution to the general public.
These pages also offer a form you can use to sign up for email updates about COVID-19 that will come immediately and directly to your inbox.
Study to Tackle Barriers to COVID-19 Testing in Black Communities
November 30, 2020
Strategies to increase COVID-19 testing in underserved black communities, to be studied by Pennington Biomedical scientists via a federal grant announced today, will also help shape COVID-19 vaccine and treatment distribution plans to citizens living in vulnerable, high-risk neighborhoods.
Baton Rouge area community partners including the Mayor President’s HealthyBR initiative and members of the Louisiana Clinical and Translational Science Center (LA CaTS) have joined the project to assist research implementation. They aim to strengthen the data on disparities in infection rates, COVID-19 testing patterns, disease progression and outcomes.
John Kirwan, Executive Director says “Getting these answers is urgent because we’re drawing ever closer to federal approval for COVID-19 vaccines and their distribution.” The study, named “Radx-UP,” is a $1.8 million NIH grant awarded to the Louisiana Clinical and Translational Science Center (LA CaTS), and Pennington Biomedical
Helpful Resources
EPA List of Antimicrobial Products
CDC Coronavirus Information
LSU Coronavirus Updates & Information
Louisiana Department of Health - Defend Against COVID-19
Louisiana Governor’s Office Coronavirus Information
PAR Research Brief: "Tracking COVID-19 Benchmarks"
Why are those with Obesity at HIgher Risk for Severe COVID-19 Infection and Death? Top 5 FAQs:
The experts at Pennington Biomedical Research Center explain why and how obesity affects COVID-19 in this FAQ. “Thank you”, for these responses goes to Steven Heymsfield, MD, FTOS, former Executive Director of the Center; Eric Ravussin, PhD, Boyd Professor and Associate Executive Director of Clinical Science, and Peter Katzmarzyk, PhD, FACSM, FTOS, Associate Executive Director for Population and Public Health Sciences.
Inflammation that often accompanies obesity can cause the body to rev up the immune system response to any infection such as COVID-19.
Under normal circumstances, inflammation indicates that the immune system is fighting off infection by sending blood cells and other messengers to the injury. Once those cells show up to the injured tissue, you’ll notice swelling and you may see a reddish or “inflamed” color. Once the wound heals, the immune system backs off, swelling goes down and color returns to normal.
In people with obesity, the immune system may see fat that surrounds organs in the abdomen, also known as visceral fat, as a threat like a potential injury. So, the immune system is working overtime sending out blood cells and other chemicals every day, all day long, to attack damaged cells. This leads to chronic inflammation.
In the case of COVID-19, the immune system goes into even higher overdrive in a way that can cause a “cytokine storm” reaction. Cytokine molecules are part of a healthy immune system response, except when the number of molecules soars. Then immune cells may build so quickly that they crowd and break through the walls of an inflamed lung, as just one result. That’s when fluids will build up in the lung, making it hard to breathe and triggering the need for ventilator support.
Roughly 40 percent of U.S. adults have obesity, which helps explain why COVID-19 is having such a big impact on our health care system.
No. It gets worse. Impaired immune systems make an individual more susceptible to viral infections in general. One study shows that adults with obesity have twice the incidence of flu or flu-like illnesses despite being vaccinated.
Obesity is also often accompanied by other conditions that are risk factors for COVID-19 complications, such as type 2 diabetes, cardiovascular disease, and pulmonary disease like obstructive sleep apnea. Obesity is also often accompanied by other conditions that are risk factors for COVID-19 complications, such as type 2 diabetes, cardiovascular disease, and pulmonary disease like obstructive sleep apnea.
Those with severe or class III obesity which is defined as a BMI of 40 or higher. A person who is 5’9” and weighs 271 pounds has a BMI of 40. A person with severe obesity who requires hospitalization presents a greater challenge. He or she may need a special, bariatric hospital bed. Even hospitals with bariatric surgery units have a limited number of these beds. Other hospitals may not have any.
People with obesity and COVID-19 are more likely to need a ventilator. But intubations may be more difficult and require personnel with specialized training. Hospitals have been able to reduce mortality rates for some patients who need ventilators by placing the patients on their stomachs. This option may not be available for people with class III obesity because they, like pregnant women, may not do well in that position.
Obtaining an imaging diagnosis may also be more complicated because many imaging machines have weight limits.
A person with obesity carries excess chest and abdominal fat, and that extra weight puts pressure on their diaphragm, lungs, and chest cavity. This can lead to breathing problems and even lung damage. In simpler terms, a person with obesity can’t get enough oxygen. He or she can’t catch a (full) breath.
It’s also possible that the extra weight may damage the diaphragm muscles. The respiratory system of a person with obesity is already laboring at a disadvantage before the added distress of a COVID-19 infection. With the infection, their blood oxygen levels could drop to near-fatal levels or fatal levels without them knowing.
Even when you skip a row, you want to go off by the number indicated in the heading column when you are setting a specific panel to open on load.
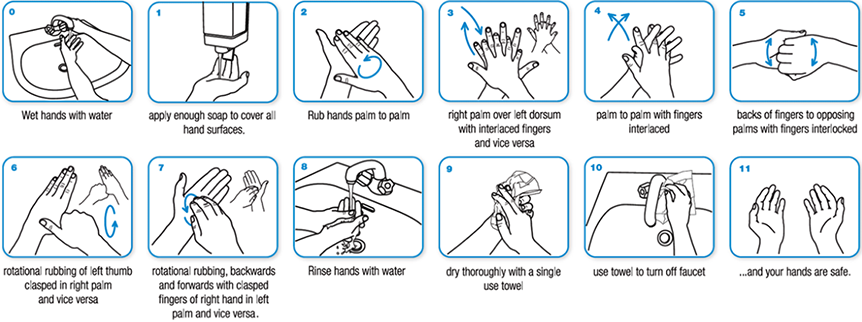
Follow the Centers for Disease Control and Prevention guidelines
- Wash your hands often with soap and water for at least 20 seconds. If soap and water aren’t available, use a hand sanitizer that’s at least 60 percent alcohol.
- Avoid close contact with people who are sick, even at home. Stay at least 6 feet away from other people outside your home. Avoid crowds and large gatherings.
- Cover your mouth and nose with a cloth face cover when around others.
- Clean and disinfect frequently touched surfaces – tables, doorknobs, light switches, countertops, etc. – every day.
- Exercise. Change your diet. Lifestyle changes, like a daily workout routine or a better diet, can help you stay healthy. Check out Pennington Biomedical’s YouTube page or follow us on Facebook and Twitter for quick tips on exercise and eating healthy.
Preventing the Spread of COVID-19
The U.S. Centers for Disease Control (CDC) has a comprehensive list of COVID-19 preventative behaviors we encourage you to review. A vaccine is not currently available for COVID-19 and everyday prevention measures are the most important steps we can take to safeguard everyone’s health.
We are asking you to make practicing appropriate hand hygiene a priority by:
- Washing your hands thoroughly with soap* and water at frequent intervals throughout the day
Additional Recommended Steps You Can Take
- Covering your coughs
- Limiting close contact with others
- Disinfecting shared common objects
- Avoid touching your face
- Avoid touching other people or attending unnecessary social interactions and travel
- Staying home if you suspect you are sick
Social Distancing Reduces Your Risk and Stops the Spread
One of the best ways to stay healthy and reduce the spread of coronavirus disease 2019 (COVID-19), is called "social distancing."
If COVID-19 is spreading in your area, limiting close contact with all individuals outside your household will help reduce the spread in your community as well.
Since people can spread the virus before they know they are sick, it is important to stay away from others when possible, even if you have no symptoms.
To Practice Social Distancing
- Stay at least 6 feet (2 meters) from other people
- Do not gather in groups
- Stay out of crowded places and avoid mass gatherings
Why is social distancing so effective?
COVID-19 spreads mainly among people who are in close contact (within about 6 feet) for a prolonged period. An infected person will cough, sneeze or talk and droplets from the mouth or nose are launched into the air and land in mouths or noses of people nearby. The droplets can also be inhaled into the lungs.
For more on social distancing, including tips on how to visit the grocery store safely, and why to wear a mask in public, see the CDC website source here: https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/social-distancing.html
Wearing a Mask
The Centers for Disease Control (CDC) now recommends that everyone wear a mask in public. This will help reduce the spread of the coronavirus and keep you healthier.
People with the virus, and even those without any symptoms or idea that they might be sick, can spread the virus. If they are wearing a mask, they are less likely to spread the virus to healthy individuals. Based on previous virus research with animals and humans, we also know that viral dose exposure affects the severity of an illness. A lower viral dose exposure gives the immune system a better chance of winning against the disease. Masks can help reduce your viral dose exposure to infected air droplets.
The CDC has also provided a “DIY Mask Tutorial” video here.